The first section was about communication (being aware of your own biases, translating medical jargon, knowing your audience, etc.) The final assignment was a paper reflecting on your own birth or postpartum experience. It was a surprisingly difficult process for me. At first I thought, "oh, I'll just right about how he was High Need, and how that was difficult." But the more I wrote and the more I cried and cried as I wrote, I realized there was so much more to it. It took several months to get to place where I felt like I was being honest with myself.
I came away from this process with the realization that new mothers are not prepared for a lot of the feelings that come with having a baby, and we don't help the situation by keeping those feelings to ourselves. So in that spirit of "saying it out loud", here it is ... don't let its "academic-ness" fool you -- it's raw and real, and it still makes me cry to read it. But it's the truth, and I hope some new mom down the road comes across this and realizes she's not alone.
Mollie Hartford
Childbirth International –
Childbirth Education Certification
Communication Assignment – FINAL
DRAFT
May 12, 2013
Postpartum Experience
INTRODUCTION
The
following is a reflection on my postpartum experience after the birth of my
first child in 2011. I will outline the circumstances of my time at home with
my son during my maternity leave and my return to work; my feelings associated
with Postpartum Depression and dealing with his intense needs; the actions I
took regarding his and my own care; and what I have learned about myself and
other mothers because of my experiences. I have not had any subsequent
pregnancies since the birth described below.
DESCRIPTION
Recount
the event. What were your goals and expectations at the time?
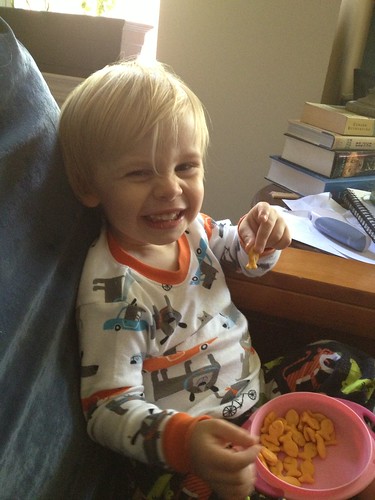
My first child, Rowan, was
born on Monday April 11, 2011. My estimated due date was April 29, so he
arrived about three weeks before I was expecting him (though at 37 weeks and
one day, he was officially full term). Not counting “pre-labor”, I was in labor
for just over 12 hours, pushing for only four minutes. I delivered at an
in-hospital birthing center in New York City, New York, USA. I had no
interventions and no medication during labor; I had no tears and required no
stitches or postpartum procedures besides a Rhogam injection. Rowan was born
healthy, weighing six pounds and four ounces and he did not require any emergency
procedures. We nursed within the first half-hour with very little help and were
both discharged after about 18 hours.
My husband, Chris, used company
sick days and vacation days in order to remain home with me for about a week; my
mother traveled from out of state to stay with us for about two weeks. After
that, I was home alone with my son until about 12 weeks postpartum, when I
returned to work full-time.
As I soon learned, Rowan was
a very “High Need” baby, though I did not know that was a diagnosis until
nearly a year later. He cried non-stop throughout the day unless I was holding
and rocking him, and then would cry uncontrollably in the evening, regardless
of whether anyone was carrying him. His screams were so loud they made my ears
ache, and whenever I met someone in hall, they would say, “Ohhhhh, you’re the
new baby on the first floor who’s always crying.” Rowan required almost
constant motion, and he was not soothed by activities like a bath or baby
massage, as those activities required setting him down. He would only sleep
lying on top of me or my husband, and would immediately wake up if we placed
him in his crib, a bed, an infant seat, a stroller, or a carseat. This meant
that it was very difficult for me to sleep at all during the day; if I tried to
lie down on the bed with him, he would wake up. I spent most of the day sitting
reclined with him resting on top of me.
We had very few problems
with breastfeeding, and he gained weight well. He nursed approximately every hour
during the day and at night, but seemed to always show some sort of hunger cue
(rooting, sucking, etc.). He progressed very quickly from first hunger cues to
crying (sometimes in less than a minute), and nursing was often the only thing
that soothed him.
We did not leave the house
very often. He cried if I put him in the stroller, and I was not confident
wearing him in the baby carrier by myself. When we did go out, he would scream
so loud and for so long that people would come up to me and ask if something
was wrong. Strangers would approach me in the street to tell me to feed him,
that he needed a pacifier, or that he needed to be burped. When I would say,
“He just cries”, they would tell me I was wrong, that he must be hungry.
Because nursing was the only thing that soothed him, it was often difficult to
maneuver outside the house; I sometimes found it difficult to find a place to
sit comfortably, and in the beginning I was not confident nursing in public or
getting him in and out of the baby carrier to nurse, so I often chose to simply
stay at home.
I
went back to work full-time at about 12 weeks postpartum, and Rowan went to a
daycare in our neighborhood. My transition back to work went well and I
continued pumping milk three times a day and sending bottles of expressed milk
to daycare. Rowan’s transition to daycare was not as easy. He did not sleep
well at daycare, and they reported that he still needed to he held when he was
awake and rocked when he was asleep, which made it difficult for the nursery
teachers to take care of the other babies. The director of the daycare would
call me to tell me he was crying so loudly that he was waking up the other
babies, or that they had to bring him up to the preschool so as not to disturb
the other babies in the nursery. They encouraged us to sleep-train him so he could
get used to falling asleep on his own.
With the exception of my
husband, very few people in my life seemed to appreciate my situation. The pediatrician
said Rowan was healthy and the crying was not considered “colic”. When I would
tell friends or co-workers that the baby was very “needy”, they would respond,
“All babies are needy” or “That’s what infants do”, and encourage us to
sleep-train him. To make matters worse, when these people would see him calm or
only crying a little, they would laugh at me and say something like, “You call
THAT crying?! That’s not even that loud!” When people would ask when we were
going to have another baby and I would say, “Never. I’m not going through this
again,” I got dismissive responses such as, “You’ll change your mind” or “It
can’t really be THAT bad”. I have even had a physician tell me, after I
admitted to being unhappy during my postpartum period, “Next time, you need to
get on antidepressants immediately. You don’t want to do that to your baby
again.” Overall, I had very little support from my friends and community.
Goals and Expectations:
Most of my conscious goals
surrounding the postpartum period were related to successful breastfeeding. I
wanted to: nurse right away in the hospital; exclusively breastfeed for at
least the first six months; delay introducing a pacifier or bottle until about
five weeks, when breastfeeding was established; pump enough milk where Chris or
a caregiver could give the baby a bottle occasionally and I could send the him
to daycare with expressed milk; and avoid supplementing with formula. While all
of these goals were met, I realize now that I also had many unconscious goals
and expectations related to my feelings toward the baby and how we would spend
our time together.
I expected to love this baby
immediately. I had imagined those first moments to be calm and beautiful, and
that I would be filled with unconditional, soul-changing love for him the
moment he was born. When we brought him home, I assumed I would be fascinated
with him. I pictured the two of us rocking quietly, me humming a lullaby and
him being content and happy. I expected that I would take him on walks around
the neighborhood, go to the park and sit quietly, or take him to run errands or
get groceries. I anticipated that when he was sleeping I could do things for
myself, like knit or read, cook for myself, or nap. I had hoped to join Mommy
& Me groups, take him to baby yoga classes, and do baby massage. I expected
to enjoy my time with him away from the office. His High Needs meant that we
could not do the quiet activities I had envisioned, and as I describe next in
the Feelings section, I did not feel the love for him that I expected.
FEELINGS
At
the time, what were you feeling? What about others? Your family, partner,
caregivers? Immediately after the event, what were you feeling? What do you
think caused these feelings?
While no one used the term “Postpartum
Depression” at the time, it was clear that I was depressed for most, if not
all, of the 12 weeks I was home with my newborn son. I was tearful and sad, had
lost interest in most things, was very anxious about leaving the house, and had
a lot of difficulty focusing on anything. I spoke to my therapist and neither
of us was worried about me harming myself or my baby, so I did not feel I
needed antidepressants, especially because I thought I would have to stop
breastfeeding. But I felt alone, both physically alone in my house, and
emotionally alone with my feelings. I have a history of depression and anxiety,
so I was not surprised to experience Postpartum Depression; I was, however,
surprised by my feelings towards my baby as well as my role as his mother.
I had many expectations for
how I would feel toward this child, and I was shocked when I did not love him
immediately. I did not even feel like his mother. I remember saying, “I must be
the best nanny in the world,” because I felt like a hired baby-nurse or wet-nurse,
a live-in nanny that also breastfed the baby. It felt as if someone had left
their baby on my doorstep, and one day they were going to come back and claim him.
I felt irrationally angry at these imaginary parents; it was unfair that they
would leave me in this situation, solely responsible for someone else’s screaming
infant but without any instructions. I felt guilty that I did not love him,
ashamed when people would ask me how things were going or make comments like
“You must love him so much, right?!” I felt like I had to lie and say that of
course I loved him, even though it took two months to even begin to feel
something that resembled love. At work, when people would ask me if it was very
difficult to be away from him, they seemed surprised when I said it was not hard
and that I was genuinely happy to be back. While other working mothers spoke
about feeling guilty for being away from their babies, I felt guilty that I was
NOT upset about being away from mine. It seemed everyone expected me to be a
mess when I returned to work, to be homesick and crying over my baby’s photos
at my desk. Instead I was excited to get back on top of my work, and it seemed
wrong that I did not miss him. When I would finally admit that he was not a
good baby or that I did not love him, people would seem shocked, and those
reactions just intensified my feeling that I was doing something wrong. Everyone
else seemed to love their baby no matter what; what was so wrong with me that I
could not love mine?
I was also embarrassed by how
much he cried. I felt like people were always staring at me when we were out
and he was screaming. I felt badgered by strangers when they told me what they
thought I was doing wrong and dismissed by my friends when they did not seem to
believe how difficult Rowan was. I was angry that when admitted I was
struggling and reached out for help I received criticism instead of support, as
if I were actively mistreating my child rather than caring for him. I felt humiliated
that I could not comfort my own son and even angry at Rowan because he never
seemed satisfied. When daycare would call to tell me he was waking the other
babies and making it hard on the teachers, I would be overcome with shame. I
thought about quitting work and keeping him at home, not because I missed him
but because at least he would not be disturbing anyone else. I felt like everyone
saw me as a bad mother because he was always so upset.
Even today, as I write this
reflection, I have tears in my eyes remembering the severity of these emotions
and the anger I feel about the reactions I received. It was not until very
recently -- nearly two years after the birth of my son -- that I have begun to
receive supportive comments from other mothers and even appreciation from other
new moms when I share my truth about those first few months. However I am still
often blindsided by the occasional negative comment. I can usually dismiss a
look of shock or an admonition from a stranger with the knowledge that my son is
thriving, and that my feelings at the time were completely natural and normal. However, there is still a part of me that
senses their judgment and I cannot help but feel that I should still be
ashamed.
ACTIONS
In
what way did your actions meet your goals? What else could you have done to
meet your goals and why didn’t you do this?
I believe I spent so much
time preparing to breastfeed and expecting breastfeeding to be difficult that I
neglected to prepare for the realistic and practical management of Postpartum Depression
(PPD). I had read several books on breastfeeding, had all the supplies I
needed, and had on-hand the contact information of all the local La Leche
League leaders and even a Lactation Consultant. All of this preparation led to
very few breastfeeding problems, quick resolutions to the minor nursing issues
we had, and a long and rewarding breastfeeding relationship. I realize now that
perhaps if I had spent more time learning about how PPD really manifests
itself, I could have dealt with those feelings more effectively. I had a
general overview of PPD from my pregnancy books – the percentage of mothers who
suffer from Postpartum Depression, how it differs from “Baby Blues” or
Postpartum Psychosis, and the symptoms. I had an overall understanding and felt
that I and my partner would be able to recognize it. Having dealt with some
bouts of depression myself, and having never taken medication for it, I assumed
that I would deal with PPD the same way: talking with my therapist, being aware
of it, and letting it pass. I expressed concerns to my therapist, and made
plans to speak with her on the phone and to come in for sessions while on my
maternity leave.
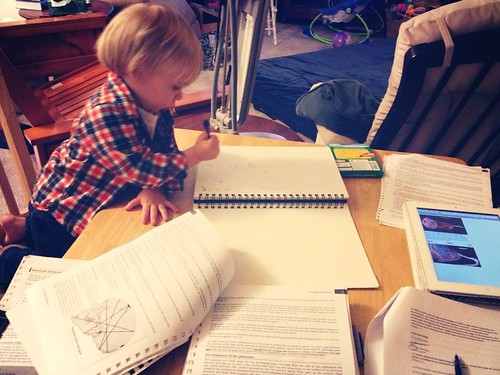
I realize now that this was
not enough preparation for me. During my maternity leave, I began reading a
book called “What Mothers Do, Especially When It Looks Like Nothing,” by Naomi
Stadlen, and at the time I remember wishing I had read it before having the
baby. The book contained quotes from mothers in support groups describing
certain aspects of motherhood, including bonding and depression. It was
tremendously comforting and validating to hear other mothers describe the same
feelings I was experiencing, and it made me aware of many of the assumptions I
had made about myself (and about motherhood in general). As I look back, I wish
I had found more references like this book, ones describing the feelings real
mothers have in an honest, nonjudgmental way. The top-line information
about PPD and the cursory statements of “there’s nothing to be ashamed of” in
the pregnancy books was not enough for me to truly understand the complexity of
the feelings or be ready for them.
I also now realize that it
was not enough to simply acknowledge that I was depressed, or to prepare my
partner to recognize that I was depressed. I should have sought out more help.
I could have spoken to my therapist more often, or I could have gone to see her
more consistently. I could have found a sitter for the baby during those
sessions so I could have focused more on the treatment. Of course, at the time,
that did not seem like a viable choice -- leaving my High Need, exclusively-breastfed
baby in the care of someone else was a very stressful thought for me.
Additionally, my partner had used all his sick time and vacation time to stay
home after the baby was born, and I felt like it was too much to ask a family
member to travel from out of state just so I could go to a doctor’s
appointment. Perhaps I could have found a PPD support group, much like the La
Leche League meetings, where I could have brought the baby and met other
mothers in my situation. Finally, while I was willing to admit that I was
tearful and sad, I never once admitted the truth that I felt like harming my
child. I knew in my heart that I would never hurt him, but still the fleeting
urges and intrusive thoughts to throw him, shake him, or let him drown
terrified me. Not only was I afraid that if I told anyone these feelings Child
Protective Services would take him away, I was worried everyone would view me
as an even worse mother than I already felt to be – not only could I not
comfort my constantly-crying child, I also wanted to hurt him. I never said
these words out loud, even to my therapist, and this only intensified feelings
of shame and isolation that most likely hindered my treatment.
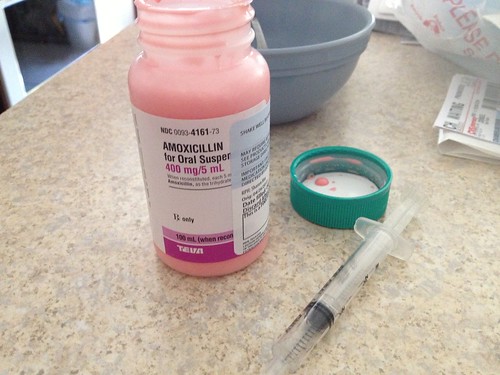
There were also a few
actions I could have taken but chose not to because I was dedicated to
breastfeeding. I could have chosen to take antidepressants to treat the
depression, but I dismissed this option immediately because I believed it meant
I would have to stop nursing. While I still do not know the specific guidelines
regarding breastfeeding while taking antidepressants, I am sure we could have
found a treatment that would have allowed continued breastfeeding. There was also
the option to transition the baby to formula, which could have led to more
sleep, more help from my partner or outside caregivers, and potentially less
social isolation. Again, I dismissed this option immediately because a
successful breastfeeding relationship and my goal to avoid formula were more
important to me than treating PPD.
Finally, I believe I could
have dealt with my child’s High Need temperament more effectively had I known
more about it. I did not know that “High Need” was a diagnosis until about a
year after he was born, and I remember asking, “Why didn’t anyone tell me?!” Much
like reading about other mothers’ postpartum feelings, learning of the
characteristics of a High Need baby was immensely comforting; I finally felt
validated in my feelings about how difficult my child had been. My therapist remembers
mentioning to me that he seemed High Need, which makes me think that I either
had not understood what she meant, or that I was so overwhelmed with my situation
that I was not really listening to her. Again, perhaps if I had made myself
available for more therapy and found alternate care for the baby during our
sessions, I could have heard her recommendations and sought support and
guidance in dealing with his needs. I do not think I would have changed much
about how I had cared for him had I known the term “High Need”, as we were
already following many of the recommendations for High Need babies (breastfeed
on demand, wear him in a baby carrier, etc.), but I believe my attitude would
have changed towards the baby had I been able to pinpoint our difficulties. Perhaps
I would not have been so bothered by his constant nursing but instead would
have realized it was exactly the comfort he needed; I would not have been as
embarrassed by his constant crying, but rather I would have seen it as simply
part of his personality and not as a reflection on my skills as a mother.
LEARNING
What
do you feel now, looking back at the event? If your feelings have changed, how
have they changed and why do you think that is? What have you learned about
yourself and others as a result of this experience and the way you have chosen
to feel about it?
I believe that the greatest
issue I had with my postpartum experience was that even after months of
preparing for this child, I was unprepared for my feelings and the limited
social support available to me. I was not the slightest bit prepared for the overwhelming
desperation I felt, the fleeting, terrifying urges I had to hurt him, or the
social stigma I felt when I tried to seek help. I thought I had been prepared
for depression, ready to recognize symptoms and seek help. I had not been
prepared for how difficult it would be to bond with my child, especially
considering I had complication-free birth, breastfeeding was going well, and
neither of us had any problems that required us to be separated. I was
surprised and disappointed by the reactions of my friends and community, who
seemed dismissive or shocked by my struggles. I was left feeling alone with the
certainty that these feelings were abnormal and that there was something wrong
with me for feeling them.
The more I speak about my
postpartum experiences, the more confident I am that my feelings were normal,
natural, and probably more pervasive than we, as a society, are willing to
admit. Reading the Childbirth International training manual’s section of
Postpartum Depression was especially eye-opening, as it described perfectly how
I had been feeling. I can now tell people that I had Postpartum Depression
(though sometimes those words are difficult to say), and I can even say that I
did not feel love for my child for the first two months of his life. Just this
morning, I joined an online discussion about the feelings associated with going
back to work full-time, saying that I believe going to work actually helped my
PPD, as it gave me an opportunity to be away from my child and excel at
something else. Still, there is always a moment after speaking these words when
I crave someone else’s approval; I still dread a shocked and judgmental
response and feel relieved when I see the reply of “Me too!” As confident as I
am in how I have raised my child so far, there is still part of me that guards
this part of our experience, fearing society’s continued judgment of me that I
did not try hard enough to be a better mother.
I believe there is an issue with
how PPD is explained to mothers. While pregnancy books include a paragraph
about PPD, our doctor’s warn us about “baby blues”, and the hospital makes us
sign a form saying we promise not to shake the baby when he cries, mothers
today are not prepared for the real feelings that can accompany having a
newborn. We do these mothers a great disservice by not being honest about our
feelings or by keeping them quiet. The only acceptable response to “How is the
baby?” seems to be “Great!” with a big smile and a hug and kiss for the child;
an honest response of “I haven’t slept more than 20 minutes in the last 5 weeks
and I want to drown him in the bathtub” is regarded as either comical or
warranting a call to Child Protective Services. We are not honest with each
other about the very real feelings of absolute desperation, so when these
feelings arise, it is no wonder we begin to question our own maternal value. As
someone who works in the TV industry, I know first-hand how motherhood is
portrayed on TV and in movies. Picture a woman, perhaps ambivalent about her
pregnancy, delivering a baby. The doctor hands her the baby and everything else
falls away. She and her baby lock eyes, and she forgets her past life and
immediately embraces her role as a mother. She instantly loves the baby, would
die before letting anything happen to it, and feels that this child is the best
thing that ever happened to her. I hate to admit it, but this picture-perfect image
is burned in my brain as reality, and I believe some of the shock of not
feeling immediately connected to my baby was due to my desire to be just like
the characters in those scenes. I grew up with these archetypes and, I am sad
to say, they are my role-models for how mothers should act, because I did not
see any alternatives in the media. We do not see real bonding struggles on TV;
we do not see real Postpartum Depression in popular movies; imagine the
backlash if Kate Middleton (or some other new-mom celebrity) gave an interview after
her baby was born and said she did not love him – she would be portrayed as a
monster.
While not every mother
experiences Postpartum Depression, I believe we owe it to each other to be
honest about our feelings, so that every mother is prepared for the possibility
of these feelings. If all we ever see is happy mothers, content babies, and
stories of tummy time and sleeping through the night, we cannot expect to know
how to handle a needy child or our own ambivalent feelings. And the more we
talk about our real feelings, the more socially acceptable these feelings will
become, and the more comfortable future mothers will be to seek help.
SUMMARY
Before writing this reflection, I was unaware of the
power these feelings of anger and shame still had on me. I believed I had moved
on and was completely comfortable discussing Postpartum Depression and my own
experiences. However, as I began writing and the tears came, I realized just
how painful these memories still are. I appreciated that I still need to
process the feelings before I can really move on and before I can confidently
teach about the subject. I know now how important it was for me to be prepared
for these feelings, and I feel that that knowledge will make me a better
teacher and a better support-person for women in my life. I know how it feels
to have my emotions dismissed, and I know how long it has taken to recover from
that treatment. I believe I can truly help other women in this situation
because I have been there and I can be the one to validate their feelings and
help them understand that they are not alone.